November — Lung Cancer Awareness Month — is being used by oncologists to stress that lung cancer can affect non-smokers as well as smokers. Physicians interviewed by the Times of India say air pollution, secondhand smoke and inherited genetic risks are driving more diagnoses among people who never smoked. Early symptoms often mimic common, mild respiratory problems — a persistent cough, breathlessness or fatigue — and are frequently ignored. Doctors urge prompt evaluation and, for high‑risk adults, consideration of low‑dose CT screening because early detection markedly improves outcomes.
Key Takeaways
- November is Lung Cancer Awareness Month; specialists are promoting vigilance for subtle symptoms and wider public education.
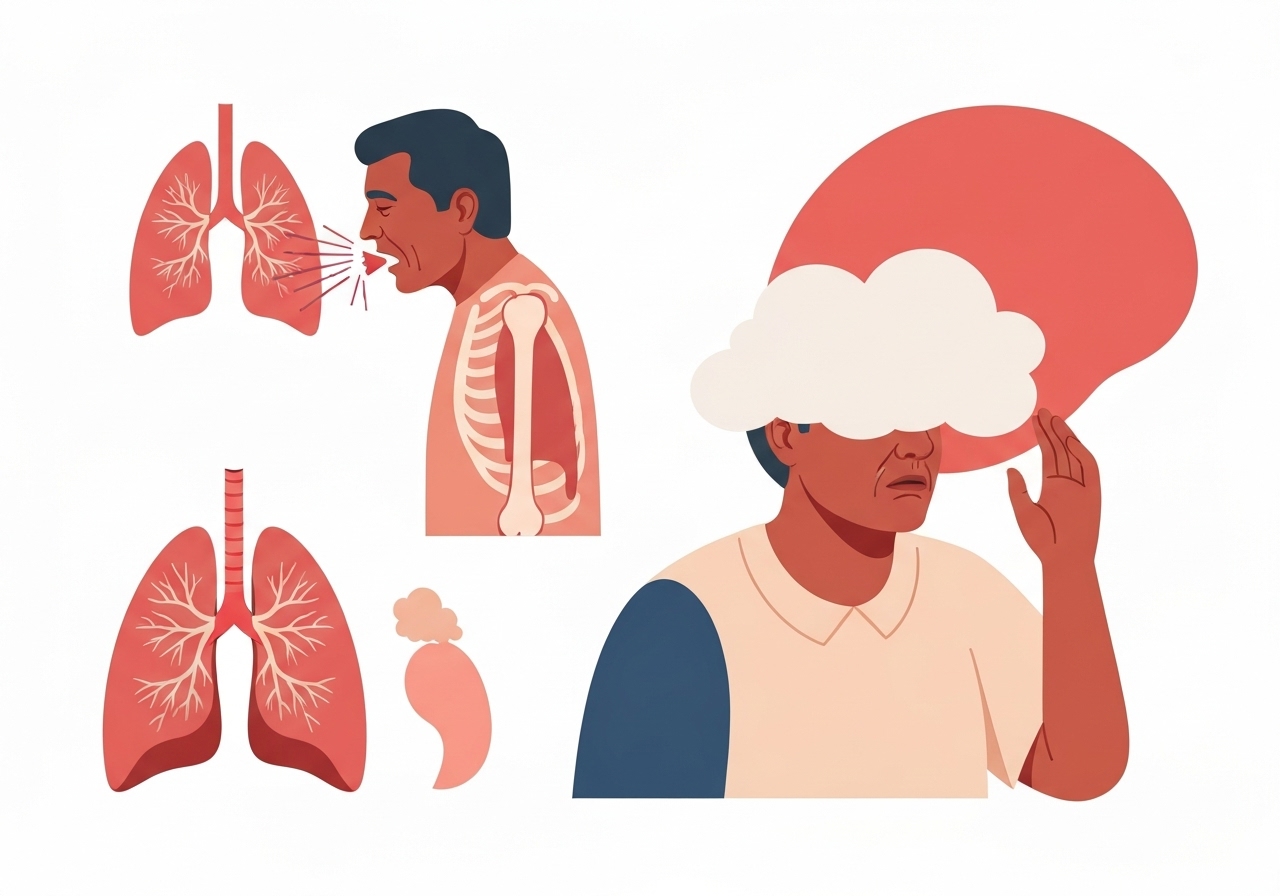
- Early warning signs include a cough lasting more than three weeks, unexplained shortness of breath, hoarseness, recurrent chest infections and traces of blood in sputum.
- Smoking remains the leading risk factor, but air pollution, secondhand smoke and genetic susceptibility are important causes in non‑smokers.
- Clinicians recommend annual low‑dose CT screening for people aged 50–80 with a history of heavy smoking; testing decisions should be individualized.
- Quitting smoking reduces risk progressively; doctors emphasize lifestyle measures — clean air, nutrition, exercise — to aid lung recovery.
- Simple measures such as improved home ventilation, vaccines against respiratory infections, and mask use on high‑pollution days can lower risk.
Background
Lung cancer is widely perceived as primarily a smoker’s disease, a perception that has shaped public messaging and screening programs for decades. That framing remains partly true — tobacco smoke contains numerous carcinogens that damage lung DNA and account for the majority of cases — but it understates other drivers. Rising urban air pollution, occupational exposures, prolonged secondhand smoke and inherited genetic traits account for a growing share of diagnoses among never‑smokers, particularly in densely populated regions.
Screening guidelines historically targeted older, long‑term smokers because that group has the highest measured risk; low‑dose CT was shown to reduce mortality in trials among heavy smokers. Public health experts now contend that awareness campaigns should also highlight non‑smoker risk factors so clinicians and patients do not dismiss early respiratory symptoms. In many parts of the world, including India, access to screening and early diagnostic services remains uneven, which complicates early detection efforts.
Main Event
Times of India spoke with two surgical oncologists about signs, prevention and screening. Dr Anadi Pachaury, Associate Director & Unit Head, Surgical Oncology at Max Super Speciality Hospital, Shalimar Bagh, described the typical early presentations he sees in clinic: lingering coughs, subtle breathlessness during routine activity and unexplained fatigue. He emphasized that even small amounts of blood in sputum warrant immediate medical review rather than being dismissed as a minor issue.
Dr Arun Kumar Goel, Chairman of Surgical Oncology at Andromeda Cancer Hospital, outlined practical thresholds for concern: a cough persisting beyond three weeks, repeated chest infections, voice changes or unexpected weight loss. Both clinicians urged that smokers and people living in high‑pollution areas be especially attentive and discuss screening with their physicians. They reiterated that quitting smoking remains the single most effective individual action to reduce long‑term risk.
The doctors recommended a combination of public education, routine primary‑care questioning about persistent chest symptoms, and targeted use of low‑dose CT for those who meet risk criteria. They also advised vaccination against influenza and pneumococcal disease as supportive measures to reduce respiratory complications that can mask or delay a cancer diagnosis. Practical home steps — air purifiers, better ventilation and avoiding indoor biomass smoke — were highlighted for people in polluted settings.
Analysis & Implications
The message that lung cancer affects non‑smokers as well as smokers has significant policy and clinical implications. If a larger proportion of cases arise in never‑smokers due to pollution and other factors, screening and public‑health strategies focused solely on smokers will miss opportunities for earlier diagnosis. Expanding clinician training to recognize subtle, persistent respiratory symptoms and improving access to diagnostic imaging could shift detection toward earlier, more treatable stages.
For individuals, the clinical implications are clear: avoid tobacco, reduce exposure to polluted air where possible, and seek evaluation for persistent respiratory symptoms. Population‑level measures are more complex and costly — improving urban air quality, enforcing workplace protections, and reducing household air pollution require coordinated policy action and investment. Yet such measures yield broad benefits beyond cancer prevention, lowering rates of chronic respiratory disease and cardiovascular illness as well.
The economics of screening are nuanced. Low‑dose CT screening reduces mortality in high‑risk groups, but its cost‑effectiveness depends on accurate selection of participants, availability of follow‑up diagnostic services, and systems to minimize harms such as overdiagnosis. In low‑resource settings, prioritizing smoking cessation programs and pollution control may offer larger population health gains than expanding imaging access alone, though both approaches are complementary.
Comparison & Data
| Risk Factor | Typical Recommendation |
|---|---|
| Current or heavy former smoker | Discuss annual low‑dose CT if aged 50–80 and meets smoking history criteria |
| Non‑smoker with pollution or secondhand exposure | Reduce exposure, improve indoor air quality, seek assessment for persistent symptoms |
| Ex‑smoker | Remain abstinent, maintain healthy lifestyle, consider periodic checks with clinician |
The table summarizes practical actions tied to common risk categories described by the clinicians. Decisions about imaging and screening should be individualized and made in consultation with a physician, taking into account age, smoking history, comorbidities and local availability of diagnostic services.
Reactions & Quotes
Clinicians framed the issue as both a clinical and public‑health challenge, urging vigilance without alarm.
“A cough that lingers for weeks or any trace of blood in sputum should prompt medical evaluation rather than being ignored,”
Dr Anadi Pachaury, Max Super Speciality Hospital (Surgical Oncology)
Dr Goel underscored the role of prevention and follow‑up.
“Quitting smoking is the most powerful preventive step, and people with heavy past smoking should discuss low‑dose CT scans with their doctor,”
Dr Arun Kumar Goel, Andromeda Cancer Hospital (Surgical Oncology)
Unconfirmed
- Exact proportion of recent lung cancer diagnoses attributable specifically to air pollution versus genetic or other causes remains an active research question and varies by region.
- Claims that lung cancer rates among never‑smokers are rising uniformly across all populations are not yet fully verified; trends differ by geography, age and exposure patterns.
Bottom Line
Lung Cancer Awareness Month serves as a timely reminder that lung cancer is not confined to current smokers. Early symptoms are often mild and easily dismissed — a persistent cough, breathlessness or fatigue — yet early evaluation can change outcomes. Clinicians recommend that people, particularly those aged 50–80 with a heavy smoking history, discuss low‑dose CT screening and that everyone adopt measures to reduce exposure to tobacco smoke and air pollution.
On an individual level, quitting smoking, maintaining good nutrition and exercise, staying current with respiratory vaccines, and seeking prompt medical assessment for persistent symptoms are practical steps that lower risk and improve recovery. At a population level, addressing air quality, workplace exposures and access to diagnostic care will be essential to reduce lung cancer’s burden beyond the smoker‑centred narrative.
Sources
- Times of India — Media report including interviews with treating oncologists.
- Max Super Speciality Hospital — Official hospital site (institutional).
- Andromeda Cancer Hospitals — Official hospital site (institutional).